NEWS
Biomedical Engineering professor and team develop treatment for traumatic brain injury
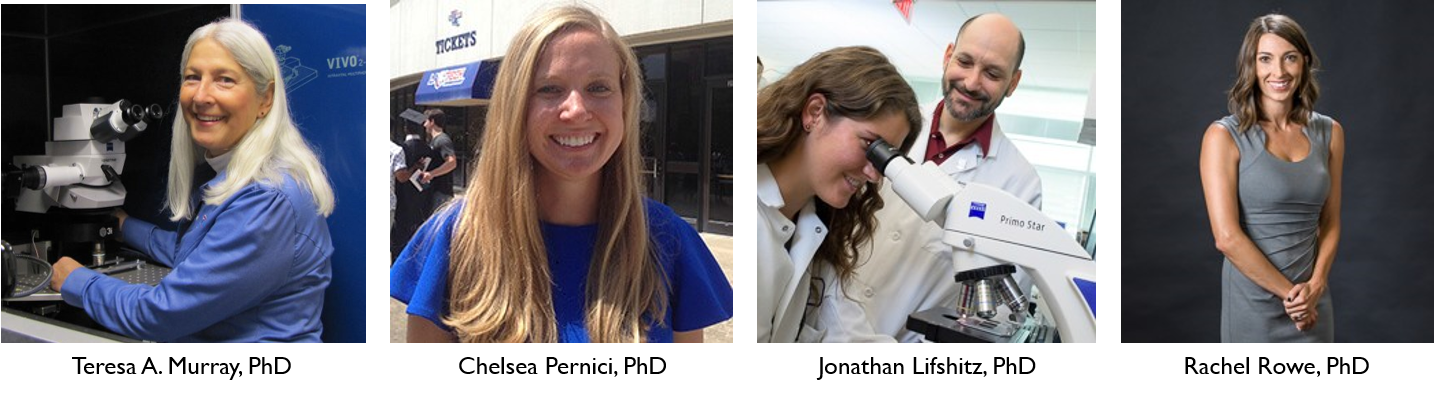
Dr. Teresa Murray, associate professor in Biomedical Engineering and the Center for Biomedical Engineering and Rehabilitation Sciences at Louisiana Tech University, is collaborating with former Louisiana Tech doctoral student Dr. Chelsea Pernici and professors at the University of Arizona to help develop solutions to traumatic brain injury.
Murray and Pernici are working with Dr. Jonathan Lifshitz and Dr. Rachel Rowe, director and research assistant professor, respectively, with the Translational Neurotrauma Research Program at the University of Arizona College of Medicine – Phoenix, to develop a treatment that could prevent memory and emotional problems in patients suffering from axonal injury caused by traumatic brain injuries (TBIs).
The study was led by Murray and Pernici who used a new imaging technology to show how diseases and injuries affect the brain over time and how medicines could reduce brain damage. This novel imaging was created in Murray’s lab. Through this technology, the group of researchers were able to repeatedly image the same axons in the brain before and after brain injury, providing proof of TBI-related axonal pathology.
Using a novel combination of high-resolution imaging and a GRIN lens implanted in the brain of mice, the team documented axonal injury and the recovery process after a blunt injury to the brain. GRIN lenses are microscopic glass lenses that allow scientists to focus closely on the cells for good image quality. These lenses are smaller than Lincoln’s nose on a U.S. penny and were adopted by a handful of biologists to better study the brain.
Murray developed an improved GRIN lens system to see more details of brain cells. Her team also designed 3D-printed hardware to help them find the exact same cells for each imaging session. Her improved GRIN lenses allowed the team to find and evaluate the same injured axons over several weeks post injury.
“The fine communication elements of neurons — axons — are torn, ruptured and damaged, which contributes to a multitude of clinical symptoms,” Lifshitz said. “To date, these processes have been inferred from fixed histological sections, clinical imaging and cells in culture. No one has observed an axon prior to injury, the consequence of injury and the outcome. Here, we show that axons do sustain injury and can either recover or become truncated.”
Tracking the time in which axons become affected, the team employed a clinically approved drug, minocycline, to reduce inflammation, which slowed axon injury, recovered them from injury and preserved function. The team tested the drug’s effectiveness for immediate use within 45 minutes of the incident, compared to delayed use at three days post injury – both time points showed positive effects. The minocycline drug treatment promoted the recovery of injured axons. With treatment, a much larger percentage of the damaged axons healed, compared to those without treatment.
“Most brain injuries cause damage to just a few axons,” Murray said. “These few axons can’t be seen on MRIs and CT scans. So, most TBI patients are sent home with the hope that they will get better over time. However, even a few damaged axons can disrupt communication in the brain and affect neurological function.”
“The novel fluorescence imaging method using GRIN lenses allows researchers to study brain cells in both time and space, offering a unique opportunity to better understand the effect of drugs on brain structure over time,” Pernici added. “It’s exciting to see that although axons become damaged after TBI, the injury can resolve and with this method, we have the opportunity to better understand that timescale.”
The team plans to continue their research by pairing minocycline with another drug to further reduce this early damage. If successful, this treatment could lessen the chances of memory loss and emotional problems for people suffering a TBI.
“This study provides hope that we can use minocycline effectively if the drug can be taken early in the process and not given long-term. This could help reduce the inflammation, and thus some of the permanent damage caused by brain injury,” Murray said.
No drug currently on the market is clinically used to prevent axon injury. The results of their research were published in Scientific Reports on May 8.